This blog post was written by special guest and expert witness:
Mr Ian Reilly, Consultant Podiatric Surgeon
Mr Reilly is a Consultant Podiatric Surgeon specialising in both the non-surgical and surgical management of foot and ankle problems. His private practice is based in the Midlands, primarily within the green county of Northamptonshire where he has performed nearly 10,000 surgical procedure.
His special interests include hallux valgus deformity (bunion), neuroma and other soft tissue pathologies of the foot & ankle.
THE BACKGROUND
A Morton’s neuroma is a common condition seen in both primary and secondary care and has gone under many names including Morton’s neuroma – the classic 3/4 interspace lesion, plantar digital neuritis, Morton’s toe, et al. Though attributed to Morton, at least two other authors could be credited with its discovery, the most famous being Durlacher who was surgeon/chiropodist to Queen Victoria.
THE CLINICAL PICTURE
We are all familiar with the typical neuroma patient: often a woman and often wearing somewhat closed-in or high heels. This typically presents as a neuralgic infliction on one foot but it can be bilateral and can affect multiple interspaces. Patients present with sharp shooting and burning neuritis, aggravated by activity and relieved by rest and massage.
THE PATHOMECHANICS
There is still quite a debate over the exact cause of the neuroma which could include stretching, compression or ischaemia of the nerve. My own view is that this is a compression neuropathy, typically with a nerve caught between adjacent proximal phalanges, occasionally metatarsal heads and occasionally the deep transverse metatarsal ligament. The common digital nerve is affected as it splits into the proper digital branches and in the 3rd interspace there is a communicating branch between the medial and lateral plantar nerve.

What does a Neuroma look like?
THE CONSERVATIVE TREATMENT
Caught early, I think there is a good argument for orthotic management and shaft padding and although it is not Rootian in thinking, I have come to recognise that the medial and lateral being between the first three medial and the two lateral metatarsals can be an issue. I am increasingly noticing that patients with Morton’s neuroma have relative hypermobility of the forefoot and in doing Mulder’s click particularly, I often see some entrapment between the adjacent medial and lateral beams of the foot.

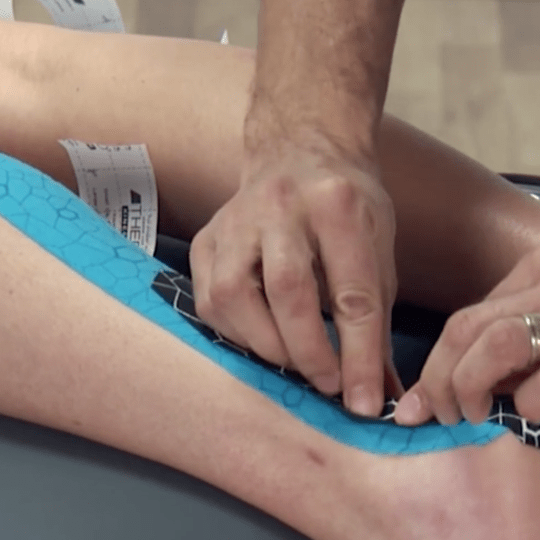
Type of insole or orthotic for a Neuroma
THE PROGNOSIS
More established cases seem to do well with cortisone shots but there is certainly a feeling in the literature that lesions below 6mm in size (if we take 2mm as a normal) tend to do better and that would certainly make sense. A smaller, less thickened, less inflamed neuroma is likely to do well with a fairly modest shot of steroid than a more established chronic and thickened neuroma.
SURGICAL PEARLS – THE PLANTAR APPROACH
Recalcitrant cases and I think this is an increasing majority of patients, go forward for surgery and there is a hot debate on whether this is a plantar or dorsal approach. I very much favour the plantar approach as this allows better visualisation of the nerve, allows the nerve to be traced back further and doesn’t do the trauma to the top of the foot in struggling to get at the nerve through an increasingly narrow interspace. I written elsewhere on this subject and presented at various conferences and this has certainly been my own experience.
Evidence based medicine which is the goal of all health professionals is not merely what seems to be the best technique as described in the literature. It is a combination of the best evidence, patient roles and practitioner experience and it is therefore a semi-scientific what works best in my hands approach. For me that is very much the plantar approach. While I have seen some painful plantar scarring the number of these has been very small and is outweighed by the number of stump neuroma I have seen – two in the last eight years.
I continue to read and reflect on my treatment of Morton’s neuroma and in fact just today came across a very good e-book written by my old friend and colleague, David Tollafield. He is a (now retired) Podiatric Surgeon of considerable experience who very recently had a Morton’s neuroma excised himself. He has done a very readable e-book aimed at the motivated patient and covers the journey in great detail and I would recommend this book to patients and practitioners alike.

Mr Reilly is a Consultant Podiatric Surgeon specialising in both the non-surgical and surgical management of foot and ankle problems. His private practice is based in the Midlands, primarily within the green county of Northamptonshire where he has performed nearly 10,000 surgical procedure.
Besides offering invasive and non-invasive services in the care of foot & problems, Mr Reilly is an experienced expert witness within the medical negligence field and has provided many a Podiatrist with training in Corticosteroid therapy, AO fixation and more recently Verruca needling. He is committed to providing the best care for his patients and contributing to the Podiatric Surgery and Podiatry profession.,
Insoles & Orthotics (Orthoses)
Insoles, also known as orthotics or orthoses, can be very effective at improving your foot alignment within your chosen shoes. This then adjusts the leg position and can help reduce the chance of injury when weightbearing by redistributing stress on affected structures and improving the efficacy of your walking or running pattern.
At OsteoGait Podiatry we provide fully customised specialist orthotics for the average walker, part-time runner to the elite Premier League footballer (more information). Additionally, we commonly utilise Corticosteroid therapy should this approach fail to improve symptoms.